

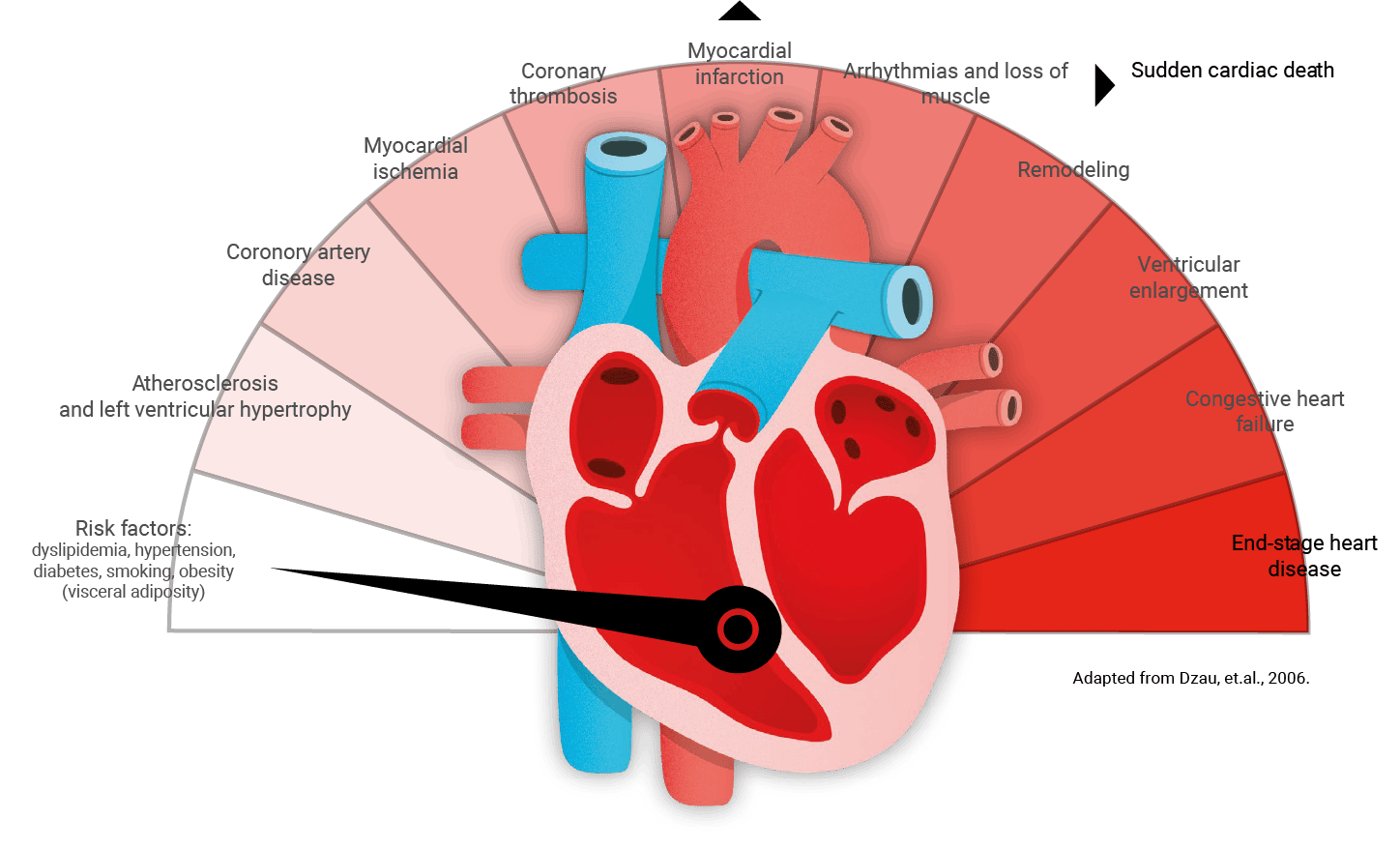
CVD continuum is a progressive process at molecular and cellular levels that manifest as clinical disease.1
Risk factors such as, elevated cholesterol, hypertension, diabetes mellitus, and cigarette smoking, are now known to promote oxidative stress and cause endothelial dysfunction, initiating a cascade of events.1
CVD should be considered as a “continuum” from the presence of CV risk factors through the development of subclinical and overt organ damage to the occurrence of major adverse cardiovascular events (MACEs), and preventive measures could and should be adopted at each level of the continuum to delay or even interrupt this progression.2
This is due to the pathophysiology of atherosclerotic disease is complex and progressive It develops silently throughout various vascular areas long before a stenosis becomes functionally significant, or an ischemic event occurs.3
Several health conditions, lifestyle, age, and family history can increase the risk for heart disease.4
HIGH BLOOD CHOLESTEROL AND OTHER LIPIDS
3.65 million deaths globally were attributed to high
LDL-C.6
(based on updated 2021 data)
25.5% of US adults have high LDL-C (≥130 mg/dL).6
(based on 2017-2020 data)
Diabetes
An independent risk factor for CVD with estimated 80%
mortality rate & the risk of a recurrent MI event is nearly
50%.7

Responsible for 10% of all deaths from CVD.8
Male adults in US reported cigarette use every day or some days.6
(Based on 2021 data)

Female adults in US reported cigarette use every day or some days.6
(Based on 2021 data)
High school students in US used e-cigarette in the past 30 days.6
(Based on 2023 data)

Insufficient intake of fruit and vegetables is estimated to cause around 11% of ischemic heart disease deaths and about 9% of stroke deaths globally.8

The prevalence of
obesity in children and adolescents
2 to 19 years of age was
20% in 2017 to 2020.6

Global: adults
41% have a healthy weight
59% have overweight or obesity.6
(Based on 2022 data)

US: adults
29% have a healthy weight
17% have overweight or obesity.6
(Based on 2017-2020 data)

In 2010
23% of adults aged 18 years and over were insufficiently physically active.
The prevalence of physical inactivity in high-income countries (33%) was about double that in low-income countries (17%).8

6-11
years of age
of US youth


12-17
years of age
of US youth
(based on 2022 data)

The age-adjusted global death rate attributable to CVD.6
(based on updated 2021 data)

The age-adjusted US death
rate attributable to CVD.6
(based on updated 2022 data)

Stroke deaths in the United States increased by
between 2012 and 2022.6
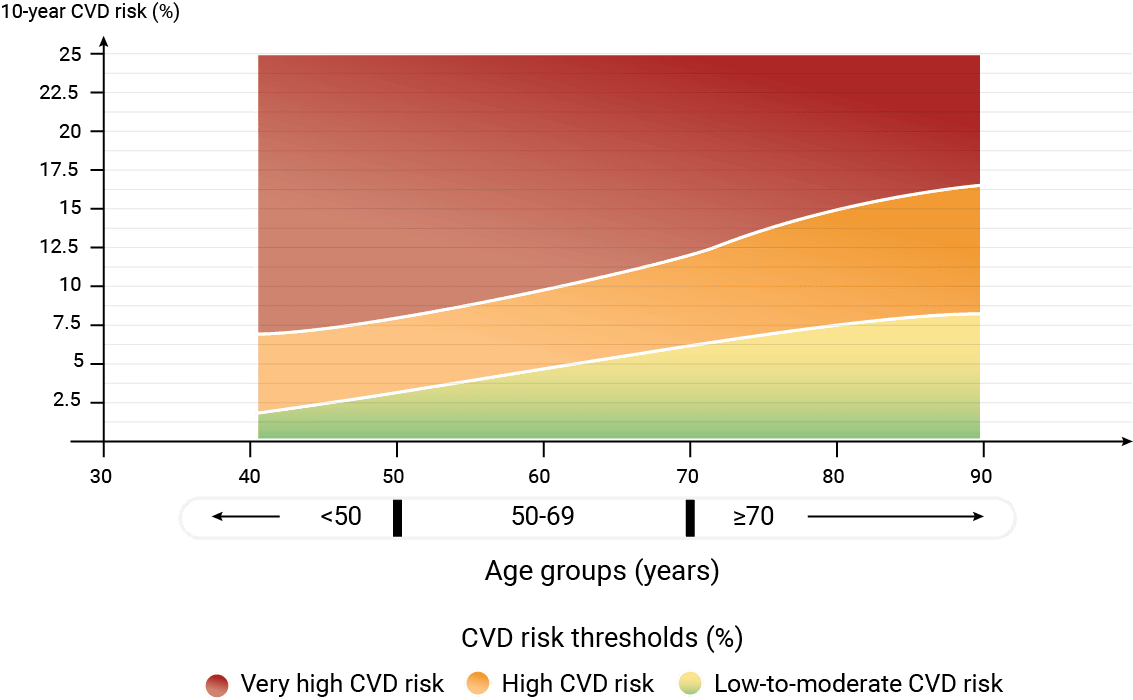
The estimation of CVD risk remains the cornerstone of ESC 2021 guidelines on CVD prevention and thus appears at the forefront of the proposed management schemes.11
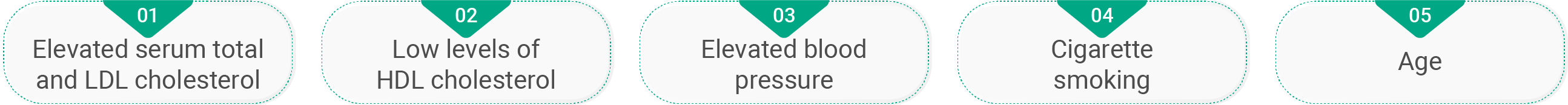
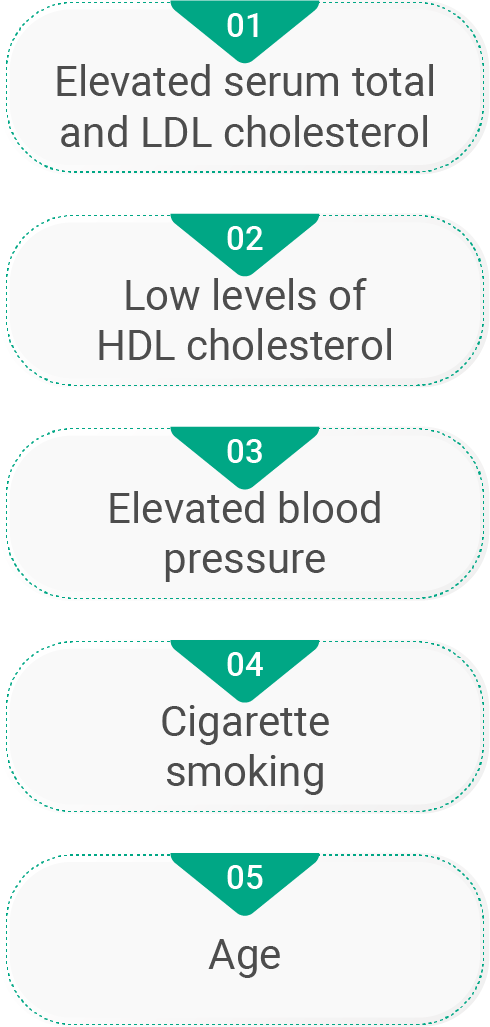
Serves as the “gold standard” in risk assessment for coronary heart disease.
The major or “traditional” risk factors identified in Framingham are well known and include
candidates for secondary prevention with diagnosed CHD or for primary prevention with vascular disease in noncoronary vascular beds, a high absolute risk (20% 10-year risk), or diabetes mellitus.
candidates for primary prevention with 2 or more risk factors and a 10-year risk of 10% to 20%.
individuals with 1 or no risk factor.
Intermediate population is best described as those with “advanced subclinical atherosclerosis”
of patients suffer an ischemic event with no measurable plaque.
of patients suffer an ischemic event with a high plaque burden but no stenosis.
of recurrent events occur in new plaques.
is a new and distinct clinical group that sits between the traditional groups of primary and secondary prevention.3
To successfully reduce the increase in CVD burden, there is a growing need to identify and manage this intermediate group of individuals with advanced subclinical atherosclerosis at the early stage.3
A clear distinction between those with primary prevention and those with advanced subclinical atherosclerosis could help encourage people to engage in lifestyle changes that would keep them from shifting into this higher-risk population.3
The ESC CVD Risk Calculation HCPs’ App provides calculators assessing individual cardiovascular risk. It includes calculators for primary and secondary prevention in various populations.
The App provides guidance to the most adapted calculator for your patient and provides an estimation of cardiovascular risk. Of note, patient data are not stored in the App.
This application is only for informative use and is not intended to provide therapeutic support or diagnosis assistance.
Is an application used to estimate a patient's initial 10-year ASCVD risk using the pooled cohort equation, receive an individualized, evidence-based, risk-guided intervention approach for managing primary prevention of ASCVD, and guide clinician-patient discussion around customizing an intervention plan.
The ASCVD Risk Estimator Plus helps clinicians implement guideline-recommended risk equations to facilitate clinician-patient discussion and support decision making to optimize care and lower risk for atherosclerotic cardiovascular disease (ASCVD).
Clinicians and patients should weigh and incorporate the information provided by this app in the context of other considerations, including recommended lifestyle interventions, patient preferences for taking medications, potential adverse drug reactions or interactions, and which treatment intervention approach might be most successful for a particular patient.
LDL-C: low denisty lipoprotein-cholesterol; CI: confidence interval; CVD: cardiovascular diseases; MI: myocardial infarction; HDL: high density lipoprotein; NCEP: national cholesterol education program; CHD: coronary heart disease; ESC: European Society of Cardiology ; US: United States; ACC: American College of Cardiology; App: application. *In a review conducted across 1,475 patients, who experienced a myocardial infarction at age ≤ 50 years.
References